Acute Gastroenteritis in Children
infections of the gastrointestinal tract caused by bacterial, viral, or parasitic pathogens
Many of these infections are foodborne illnesses
The most common manifestations are diarrhea and vomiting, which can also be associated with systemic features such as abdominal pain and fever.
Diarrheal disorders in childhood account for a large proportion (9%) of childhood deaths, with an estimated 0.71 million deaths per year globally,
Many of these infections are foodborne illnesses
The most common manifestations are diarrhea and vomiting, which can also be associated with systemic features such as abdominal pain and fever.
Diarrheal disorders in childhood account for a large proportion (9%) of childhood deaths, with an estimated 0.71 million deaths per year globally,
ETIOLOGY OF DIARRHEA
Gastroenteritis is the result of infection acquired through the fecal–oral route or by ingestion of contaminated food or water
Gastroenteritis is associated with poverty, poor environmental hygiene, and development indices.
rotavirus and the noroviruses (small round viruses such as Norwalk-like virus and caliciviruses) are the most common viral agents, followed by sapoviruses, enteric adenoviruses and astroviruses
Shigella, Salmonella, E. coli, Campylobacter are examples of bacterial causes
Giardia and Entamoeba histolytica are examples of paracytic causes
Gastroenteritis is associated with poverty, poor environmental hygiene, and development indices.
rotavirus and the noroviruses (small round viruses such as Norwalk-like virus and caliciviruses) are the most common viral agents, followed by sapoviruses, enteric adenoviruses and astroviruses
Shigella, Salmonella, E. coli, Campylobacter are examples of bacterial causes
Giardia and Entamoeba histolytica are examples of paracytic causes
PATHOGENESIS OF INFECTIOUS DIARRHEA
1- non-inflammatory diarrhea through enterotoxin production by some bacteria, destruction of villus (surface) cells by viruses, adherence by parasites, and adherence and/or translocation by bacteria
2- Inflammatory diarrhea is usually caused by bacteria that directly invade the intestine or produce cytotoxins
2- Inflammatory diarrhea is usually caused by bacteria that directly invade the intestine or produce cytotoxins
Risk factors for diarrhea
Lack of exclusive breastfeeding (0-5 mo)
No breastfeeding (6-23 mo)
Underweight,stunted,wasted(malnourished)
Vitamin A deficiency
Zinc deficiency
Crowding (>8 persons/kitchen)
Indoor air pollution
Unwashed hands
Poor water quality
Inappropriate excreta disposal
No breastfeeding (6-23 mo)
Underweight,stunted,wasted(malnourished)
Vitamin A deficiency
Zinc deficiency
Crowding (>8 persons/kitchen)
Indoor air pollution
Unwashed hands
Poor water quality
Inappropriate excreta disposal
definition
Acute diarrhea is defined as the abrupt onset of 3 or more loose stools per day and lasts no longer than 14 days
Increase frequency and/or liquidity of stool
Stool output >10 g/kg/24 hr, or more than the adult limit of 200 g/24 hr.
Increase frequency and/or liquidity of stool
Stool output >10 g/kg/24 hr, or more than the adult limit of 200 g/24 hr.
Rotavirus infection
typically begins after an incubation period of <48 hr with mild to moderate fever as well as vomiting, followed by the onset of frequent, watery stools. All 3 symptoms are present in about 50-60% of cases. Vomiting and fever typically abate during the 2nd day of illness, but diarrhea often continues for 5-7 days. The stool is without gross blood or white blood cells. Dehydration may develop and progress rapidly, particularly in infants. The most severe disease typically occurs among children 4-36 mo of age. Malnourished children and children with underlying intestinal disease, are particularly likely to acquire severe rotavirus diarrhea
Shigella
Four species of Shigella are responsible for bacillary dysentery:
S. dysenteriae
S. flexneri
S. boydii
S. sonnei
S. boydii
S. sonnei
It is most common in the 2nd and 3rd year of life, infection in the 1st 6 mo of life is rare (may be due to Breast feeding)
The colon is the target organ for shigellae
Symptoms:
generalized toxicity
urgency, and painful defecation characteristically occur.
watery → bloody mucoid stools
Convulsions, headache, lethargy, confusion, nuchal rigidity, or hallucinations may be present before or after the onset of diarrhea.
Escherichia Coli :
gram-negative bacilli
5 major groups of diarrheagenic E. coli:
(1) enterotoxigenic E. coli (ETEC)
(2) enteroinvasive E. coli (EIEC)
(3) enteropathogenic E. coli (EPEC)
(4) Shiga toxin–producing E. coli (STEC)also known
as enterohemorrhagic E. coli (EHEC)
(5) enteroaggregative E. coli (EAEC).
5 major groups of diarrheagenic E. coli:
(1) enterotoxigenic E. coli (ETEC)
(2) enteroinvasive E. coli (EIEC)
(3) enteropathogenic E. coli (EPEC)
(4) Shiga toxin–producing E. coli (STEC)also known
as enterohemorrhagic E. coli (EHEC)
(5) enteroaggregative E. coli (EAEC).
Giardia Lamblia
• It infects the duodenum and small intestine
• Clinically: asymptomatic, acute infectious diarrhea (insidious onset of progressive anorexia, nausea, gaseousness, abdominal distention, watery diarrhea) or chronic diarrhea with persistent GIT signs and symptoms, including FTT and abdominal pain or cramping.
• There is usually no extraintestinal spread.
• Clinically: asymptomatic, acute infectious diarrhea (insidious onset of progressive anorexia, nausea, gaseousness, abdominal distention, watery diarrhea) or chronic diarrhea with persistent GIT signs and symptoms, including FTT and abdominal pain or cramping.
• There is usually no extraintestinal spread.
Entamoeba histolytica
• Clinical presentations range from asymptomatic cyst passage to amebic colitis, amebic dysentery, ameboma, and extraintestinal disease as amebic liver disease.
• Amebic colitis, gradual onset of colicky abdominal pains and frequent bowel movements (6–8/day). Diarrhea is frequently associated with tenesmus. Stools are blood stained and contain a fair amount of mucus with few leukocytes. Generalized constitutional symptoms and signs are characteristically absent, with fever documented in only ⅓ of patients.
• Amebic colitis, gradual onset of colicky abdominal pains and frequent bowel movements (6–8/day). Diarrhea is frequently associated with tenesmus. Stools are blood stained and contain a fair amount of mucus with few leukocytes. Generalized constitutional symptoms and signs are characteristically absent, with fever documented in only ⅓ of patients.
Clinical Evaluation of Diarrhea
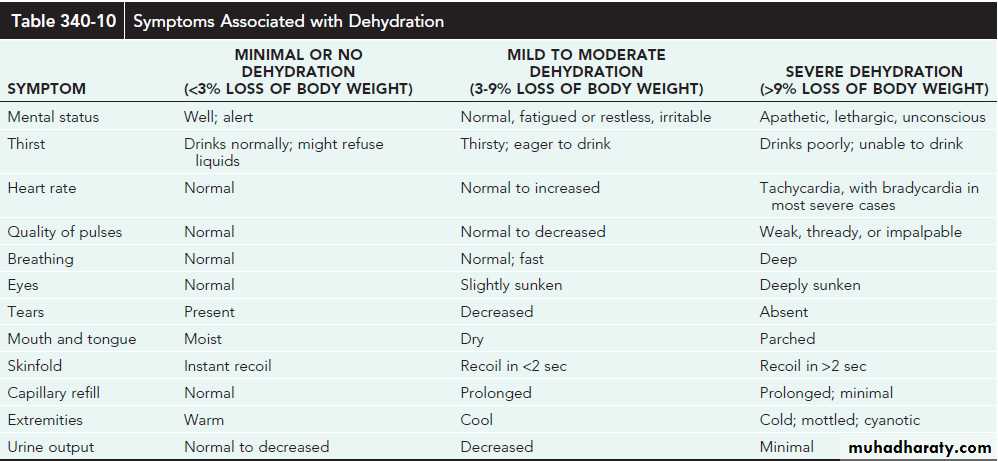
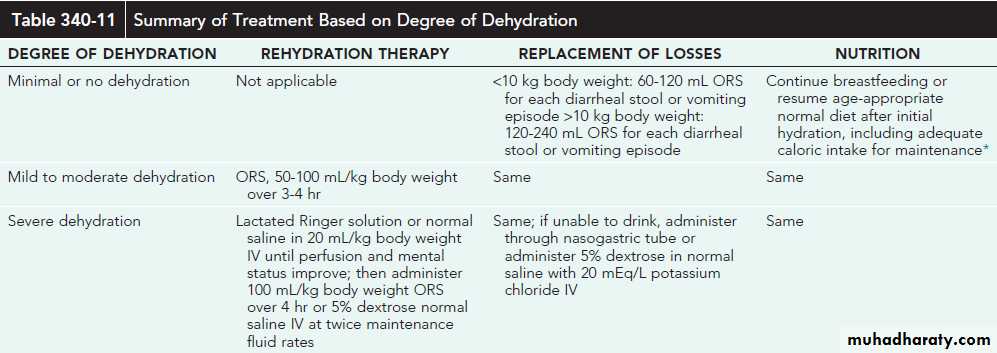
1- Assessing the degree of dehydration and acidosis and provide rapid resuscitation and rehydration with oral or intravenous fluids as required
2- Clinically determining the etiology of diarrhea for institution of prompt antibiotic therapy, if indicated
2- Clinically determining the etiology of diarrhea for institution of prompt antibiotic therapy, if indicated
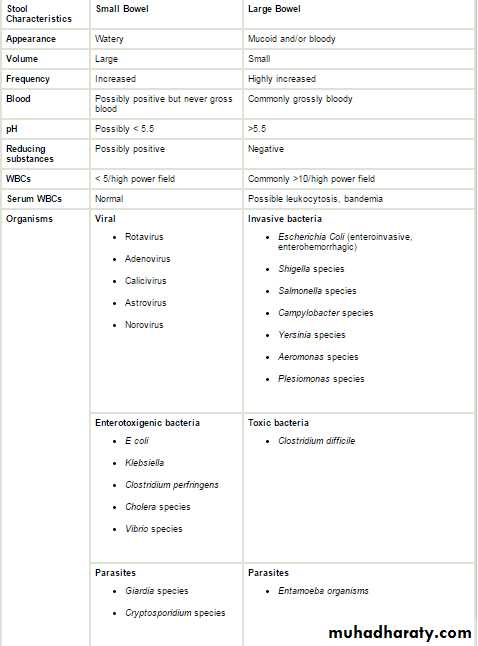
Stool characteristics (eg, consistency, color, volume, frequency)
Presence of associated enteric symptoms (eg, nausea/vomiting, fever, abdominal pain)
Use of child daycare (common pathogens: rotavirus, astrovirus, calicivirus;Campylobacter, Shigella, Giardia, and Cryptosporidium species [spp])
Food ingestion history (eg, raw/contaminated foods, food poisoning)
Water exposure (eg, swimming pools, marine environment)
Camping history (possible exposure to contaminated water sources)
Travel history (common pathogens affect specific regions; also consider rotavirus and Shigella, Salmonella, and Campylobacter spp regardless of specific travel history, as these organisms are prevalent worldwide)
Animal exposure (eg, young dogs/cats: Campylobacter spp; turtles:Salmonella spp)
Predisposing conditions (eg, hospitalization, antibiotic use, immunocompromised state)
Although nausea and vomiting are nonspecific symptoms, they indicate infection in the upper intestine.
Fever suggests an inflammatory process(inflammatory diarrhea) but also occurs as a result of dehydration or coinfection (e.g., urinary tract infection, otitis media)called also parenteral diarrhea(etiology outside the G.I system)
Severe abdominal pain, tenesmus and bloody diarrhoea indicate involvement of the large intestine and rectum.
Features such as nausea and vomiting and absent or low-grade fever with mild to moderate periumbilical pain and watery diarrhea indicate small intestine involvement and also reduce the likelihood of a serious bacterial infection.
Use of child daycare (common pathogens: rotavirus, astrovirus, calicivirus;Campylobacter, Shigella, Giardia, and Cryptosporidium species [spp])
Food ingestion history (eg, raw/contaminated foods, food poisoning)
Water exposure (eg, swimming pools, marine environment)
Camping history (possible exposure to contaminated water sources)
Travel history (common pathogens affect specific regions; also consider rotavirus and Shigella, Salmonella, and Campylobacter spp regardless of specific travel history, as these organisms are prevalent worldwide)
Animal exposure (eg, young dogs/cats: Campylobacter spp; turtles:Salmonella spp)
Predisposing conditions (eg, hospitalization, antibiotic use, immunocompromised state)
Although nausea and vomiting are nonspecific symptoms, they indicate infection in the upper intestine.
Fever suggests an inflammatory process(inflammatory diarrhea) but also occurs as a result of dehydration or coinfection (e.g., urinary tract infection, otitis media)called also parenteral diarrhea(etiology outside the G.I system)
Severe abdominal pain, tenesmus and bloody diarrhoea indicate involvement of the large intestine and rectum.
Features such as nausea and vomiting and absent or low-grade fever with mild to moderate periumbilical pain and watery diarrhea indicate small intestine involvement and also reduce the likelihood of a serious bacterial infection.
InvestigationS
1-Stool Examination
A-Microscopic examination of the stool: Fecal leukocytes and RBC indicate bacterial invasion of colonic mucosa, stool microscopy must include examination for parasites causing diarrhea, such as G. lamblia and E. histolytica
B- Stool culture is required if the child appears septic, if there is blood or mucus in the stools or the child is immunocompromised.It may be indicated following recent foreign travel, if the diarrhoea has not improved by day 7 or the diagnosis is uncertain
3- Plasma electrolytes, urea, creatinine and glucose should be checked if intravenous fluids are required or there are features suggestive of hypernatraemia.
4- If antibiotics are started, a blood culture should be taken.
5- urinalysis to exclude UTI (parenteral diarrhea)
6- Enzyme immunoassay for rotavirus or adenovirus antigens
A-Microscopic examination of the stool: Fecal leukocytes and RBC indicate bacterial invasion of colonic mucosa, stool microscopy must include examination for parasites causing diarrhea, such as G. lamblia and E. histolytica
B- Stool culture is required if the child appears septic, if there is blood or mucus in the stools or the child is immunocompromised.It may be indicated following recent foreign travel, if the diarrhoea has not improved by day 7 or the diagnosis is uncertain
3- Plasma electrolytes, urea, creatinine and glucose should be checked if intravenous fluids are required or there are features suggestive of hypernatraemia.
4- If antibiotics are started, a blood culture should be taken.
5- urinalysis to exclude UTI (parenteral diarrhea)
6- Enzyme immunoassay for rotavirus or adenovirus antigens
BLOODY DIARRHEA
Causes of bloody diarrhoea (real or apparent) in infants and children Infants aged <1 year
1- Intestinal infection(shigella,salmonella,E-coli,campylobacter,Yersinia)
And Entamoeba histolytica
2- Infant colitis(Cow’s milk colitis)—non specific allergic colitis
3- rare causes like Intussusception, Malrotation and volvulus
1- Intestinal infection(shigella,salmonella,E-coli,campylobacter,Yersinia)
And Entamoeba histolytica
2- Infant colitis(Cow’s milk colitis)—non specific allergic colitis
3- rare causes like Intussusception, Malrotation and volvulus
Infants aged >1 year
1- Intestinal infection
2- Inflammatory bowel disease
3- Juvenile polyp
4- rare causes Intussusception , Malrotation and volvulus and Henoch-Schönlein purpura
Recent antibiotic use raises suspicion for antibiotic-associated colitis and Clostridium difficile colitis.
2- Inflammatory bowel disease
3- Juvenile polyp
4- rare causes Intussusception , Malrotation and volvulus and Henoch-Schönlein purpura
Recent antibiotic use raises suspicion for antibiotic-associated colitis and Clostridium difficile colitis.
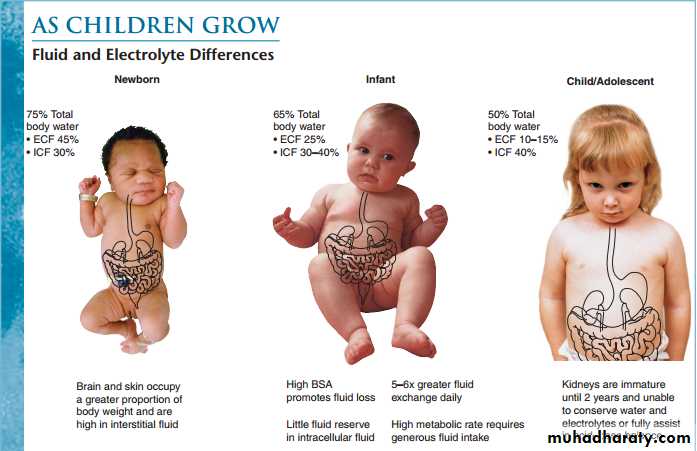
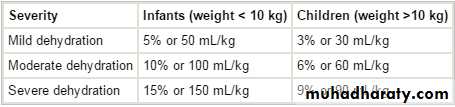
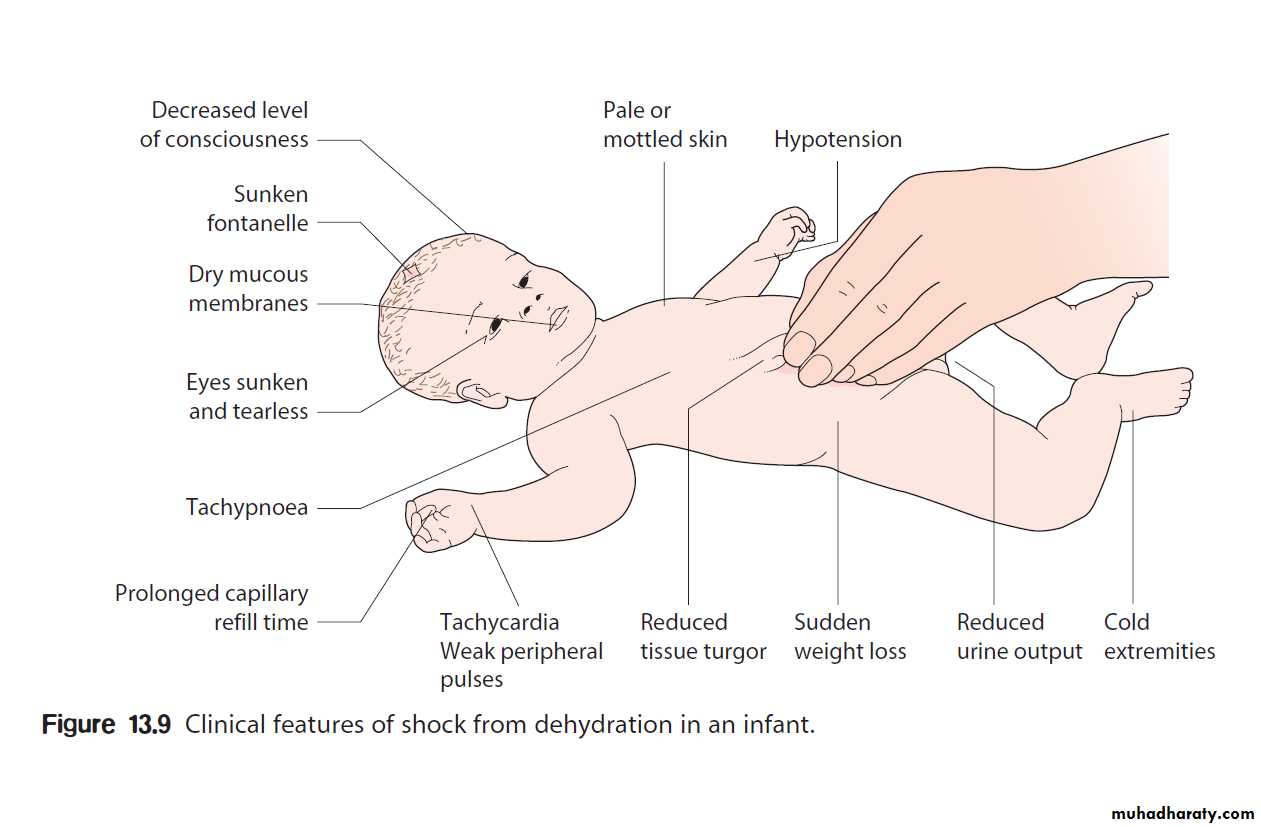
DEHYDRATION (total body deficit of sodiumand water)
The following children are at increased risk of dehydration:
Infants, particularly those under 6 months of age or those born with low birthweight.
• If they have passed ≥6 diarrhoeal stools in the previous 24 h • If they have vomited three or more times in the previous 24 h
• If they have been unable to tolerate (or not been offered) extra fluids
• If they have malnutrition
Infants are at particular risk of dehydration because they have a greater surface area to weight ratio than older children, leading to greater insensible water losses .They have higher basal fluid requirements (100–120 ml/kg per day, i.e. 10–12% of bodyweight) and immature renal tubular reabsorption. In addition, they are unable to obtain fluids for themselves when thirsty.
Infants, particularly those under 6 months of age or those born with low birthweight.
• If they have passed ≥6 diarrhoeal stools in the previous 24 h • If they have vomited three or more times in the previous 24 h
• If they have been unable to tolerate (or not been offered) extra fluids
• If they have malnutrition
Infants are at particular risk of dehydration because they have a greater surface area to weight ratio than older children, leading to greater insensible water losses .They have higher basal fluid requirements (100–120 ml/kg per day, i.e. 10–12% of bodyweight) and immature renal tubular reabsorption. In addition, they are unable to obtain fluids for themselves when thirsty.
treatment
ORS
The low-osmolality World Health Organization (WHO) oral rehydration solution (ORS) containing 75 mEq of sodium, 64 mEq of chloride, 20 mEq of potassium, and 75 mmol of glucose per liter, with total osmolarity of 245 mOsm/L, is now the global standard of care and more effective than home fluids, including decarbonated soda beverages, fruit juices, and tea. These are not suitable for rehydration or maintenance therapy because they have inappropriately high osmolalities and low sodium concentrations.
Oral rehydration should be given to infants and children slowly, especially if they have emesis. It can be given initially by a dropper, teaspoon, or syringe, beginning with as little as 5 mL at a time .The volume is increased as tolerated.
Oral rehydration can also be given by a nasogastric tube if needed; this is not the usual route.
Limitations to oral rehydration therapy include shock, an ileus, intussusception, carbohydrate intolerance (rare), severe emesis, and high stool output (>10 mL/kg/hr)
Hypernatraemic dehydration ( sodium concentration >150 mEq/L)
Infrequently, water loss exceeds the relative sodium loss and plasma sodium concentration increases (hypernatraemic dehydration). This usually results from high insensible water losses (high fever or hot, dry environment)or from profuse, low-sodium diarrhea. The extracellular fluid becomes hypertonic with respect to the intracellular fluid, which leads to a shift of water into the extracellular space from the intracellular compartment. Signs of extracellular fluid depletion are therefore less per unit of fluid loss, and depression of the fontanelle, reduced tissue elasticity and sunken eyes are less obvious. This makes this form of dehydration more difficult to recognise clinically , particularly in an obese infant.
It is a particularly dangerous form of dehydration as water is drawn out of the brain and cerebral shrinkage within a rigid skull may lead to jittery movements, increased muscle tone with hyper reflexia, altered consciousness, seizures and multiple, small cerebral haemorrhages.
If the serum sodium concentration is lowered rapidly, there is movement of water from the serum into the brain cells to equalize the osmolality in the 2 compartments . The resultant brain swelling manifests as seizures or coma.
Because of the associated dangers, hypernatremia should not be corrected rapidly. The goal is to decrease the serum sodium by <12 mEq/L every 24 hr-- The fluid deficit should be replaced over at least 48 h and the plasma sodium measured regularly
It is a particularly dangerous form of dehydration as water is drawn out of the brain and cerebral shrinkage within a rigid skull may lead to jittery movements, increased muscle tone with hyper reflexia, altered consciousness, seizures and multiple, small cerebral haemorrhages.
If the serum sodium concentration is lowered rapidly, there is movement of water from the serum into the brain cells to equalize the osmolality in the 2 compartments . The resultant brain swelling manifests as seizures or coma.
Because of the associated dangers, hypernatremia should not be corrected rapidly. The goal is to decrease the serum sodium by <12 mEq/L every 24 hr-- The fluid deficit should be replaced over at least 48 h and the plasma sodium measured regularly
Isonatraemic dehydration (sodium 135-150 meq/l)
the losses of sodium and water are proportional and plasma sodium remains within the normal range
Most common type
Most common type
hyponatraemic dehydration: (serum sodium level <135 mEq/L)
When children with diarrhoea drink large quantities of water or other hypotonic solutions, there is a greater net loss of sodium than water, leading to a fall in plasma sodium (hyponatraemic dehydration). This leads to a shift of water from extra- to intracellular compartments. The increase in intracellular volume leads to an increase in brain volume, which may result in convulsions, whereas the marked extracellular depletion leads to a greater degree of shock per unit of water loss. This
form of dehydration is more common in poorly nourished infants in developing countries.
form of dehydration is more common in poorly nourished infants in developing countries.
Severe dehydration(TREATMENT)
Phase 1 : focuses on emergency management. Severe dehydration is characterized by a state of hypovolemic shock requiring rapid treatment. Initial management includes placement of an intravenous or intraosseous line and rapid administration of 20 mL/kg of an isotonic crystalloid (eg, lactated Ringer solution, 0.9% sodium chloride). Additional fluid boluses may be required depending on the severity of the dehydration. The child should be frequently reassessed to determine the response to treatment. As intravascular volume is replenished, tachycardia, capillary refill, urine output, and mental status all should improve. If improvement is not observed after 60 mL/kg of fluid administration, other etiologies of shock (eg, cardiac, anaphylactic, septic) should be considered. Hemodynamic monitoring and inotropic support may be indicated.
Phase 2: focuses on deficit replacement, provision of maintenance fluids, and replacement of ongoing losses. Maintenance fluid requirements are equal to measured fluid losses (urine, stool) plus insensible fluid losses. Normal insensible fluid loss is approximately 400-500 mL/m2 body surface area and may be increased by factors such as fever and tachypnea.
Alternatively, daily fluid requirements may be roughly estimated as follows:
Less than 10 kg = 100 mL/kg
10-20 kg = 1000 + 50 mL/kg for each kg over 10 kg
Greater than 20 kg = 1500 + 20 mL/kg for each kg over 20 kg
Severe dehydration by clinical examination suggests a fluid deficit of 10-15% of body weight in infants and 6-9% of body weight in older children. The daily maintenance fluid is added to the fluid deficit. In general, the recommended administration is one half of this volume administered over 8 hours and administration of the remainder over the following 16 hours. Continued losses (eg, emesis, diarrhea) must be promptly replaced.
If the child is isonatremic (130-150 mEq/L), the sodium deficit incurred can generally be corrected by administering the fluid deficit plus maintenance as 5% dextrose in 0.45-0.9% sodium chloride. Potassium (20 mEq/L potassium chloride) may be added to maintenance fluid once urine output is established and serum potassium levels are within a safe range.
Phase 2: focuses on deficit replacement, provision of maintenance fluids, and replacement of ongoing losses. Maintenance fluid requirements are equal to measured fluid losses (urine, stool) plus insensible fluid losses. Normal insensible fluid loss is approximately 400-500 mL/m2 body surface area and may be increased by factors such as fever and tachypnea.
Alternatively, daily fluid requirements may be roughly estimated as follows:
Less than 10 kg = 100 mL/kg
10-20 kg = 1000 + 50 mL/kg for each kg over 10 kg
Greater than 20 kg = 1500 + 20 mL/kg for each kg over 20 kg
Severe dehydration by clinical examination suggests a fluid deficit of 10-15% of body weight in infants and 6-9% of body weight in older children. The daily maintenance fluid is added to the fluid deficit. In general, the recommended administration is one half of this volume administered over 8 hours and administration of the remainder over the following 16 hours. Continued losses (eg, emesis, diarrhea) must be promptly replaced.
If the child is isonatremic (130-150 mEq/L), the sodium deficit incurred can generally be corrected by administering the fluid deficit plus maintenance as 5% dextrose in 0.45-0.9% sodium chloride. Potassium (20 mEq/L potassium chloride) may be added to maintenance fluid once urine output is established and serum potassium levels are within a safe range.
Enteral Feeding and Diet Selection
Continued enteral feeding in diarrhea aids in recovery from the episode, and a continued age-appropriate diet after rehydration is the norm.
Once rehydration is complete, food should be reintroduced while oral rehydration is continued to replace ongoing losses from emesis or stools and for maintenance. Breastfeeding or non diluted regular formula should be resumed as soon as possible. Foods with complex carbohydrates (rice, wheat, potatoes, bread, and cereals), lean meats, yogurt, fruits, and vegetables are also tolerated
Fatty foods or foods high in simple sugars (juices, carbonated sodas) should be avoided
Once rehydration is complete, food should be reintroduced while oral rehydration is continued to replace ongoing losses from emesis or stools and for maintenance. Breastfeeding or non diluted regular formula should be resumed as soon as possible. Foods with complex carbohydrates (rice, wheat, potatoes, bread, and cereals), lean meats, yogurt, fruits, and vegetables are also tolerated
Fatty foods or foods high in simple sugars (juices, carbonated sodas) should be avoided
Zinc Supplementation
Zinc administration for diarrhea management can significantly reduce all cause mortality by 46% and hospital admission by 23%. Also reduce duration and severity of diarrhea
All children older than 6 mo of age with acute diarrhea in at-risk areas should receive oral zinc (20 mg/day) in some form for 10-14 days during and continued after diarrhea
All children older than 6 mo of age with acute diarrhea in at-risk areas should receive oral zinc (20 mg/day) in some form for 10-14 days during and continued after diarrhea
Additional Therapies
The use of probiotic nonpathogenic bacteria for prevention and therapy of diarrhea has been successful in some settings
Saccharomyces boulardii is effective in antibiotic-associated and in C. difficile diarrhea, and there is some evidence that it might prevent diarrhea in daycare centers. Lactobacillus rhamnosus GG is associated with reduced diarrheal duration and severity, which reduction is more evident in cases of childhood rotavirus diarrhea
Antimotility agents (loperamide) are contraindicated in children with dysentery and probably have no role in the management of acute watery diarrhea in otherwise healthy children.
Because persistent vomiting can limit oral rehydration therapy, a single sublingual dose of an oral dissolvable tablet of ondansetron (4 mg 4-11 yr and 8 mg for children older than 11 yr [generally 0.2 mg/kg]) may be given.However, most children do not require specific antiemetic therapy;careful oral rehydration therapy is usually sufficient.
Saccharomyces boulardii is effective in antibiotic-associated and in C. difficile diarrhea, and there is some evidence that it might prevent diarrhea in daycare centers. Lactobacillus rhamnosus GG is associated with reduced diarrheal duration and severity, which reduction is more evident in cases of childhood rotavirus diarrhea
Antimotility agents (loperamide) are contraindicated in children with dysentery and probably have no role in the management of acute watery diarrhea in otherwise healthy children.
Because persistent vomiting can limit oral rehydration therapy, a single sublingual dose of an oral dissolvable tablet of ondansetron (4 mg 4-11 yr and 8 mg for children older than 11 yr [generally 0.2 mg/kg]) may be given.However, most children do not require specific antiemetic therapy;careful oral rehydration therapy is usually sufficient.
Antibiotic Therapy
antibiotic therapy in select cases of diarrhea related to bacterial infections can reduce the duration and severity of illness and prevent complications
Although these agents are important to use in specific cases, their widespread and indiscriminate use leads to the development of antimicrobial resistance.
Although these agents are important to use in specific cases, their widespread and indiscriminate use leads to the development of antimicrobial resistance.
PREVENTION
1- Promotion of Exclusive Breastfeeding (administration of no other fluids or foods for the 1st 6 mo of life)
2- Improved Complementary Feeding Practices
3- Rotavirus Immunization
4- Improved Water and Sanitary Facilities and Promotion of Personal and Domestic Hygiene
5- Improved Case Management of Diarrhea
2- Improved Complementary Feeding Practices
3- Rotavirus Immunization
4- Improved Water and Sanitary Facilities and Promotion of Personal and Domestic Hygiene
5- Improved Case Management of Diarrhea
Complications(Extraintestinal Manifestations of Enteric Infections)
1- Focal infections from systemic spread of bacterial pathogens, includingvulvovaginitis, urinary tract infection,endocarditis, osteomyelitis, meningitis,pneumonia, hepatitis, peritonitis,chorioamnionitis, soft-tissue infection,and septic thrombophlebitis
2- Reactive arthritis
3- Guillain-Barré syndrome
4- Glomerulonephritis
2- Reactive arthritis
3- Guillain-Barré syndrome
4- Glomerulonephritis
5- Immunoglobulin A (IgA) nephropathy
6- Erythema nodosum
7- Hemolytic uremic syndrome: Escherichia coli O157:H7
8- Hemolytic anemia
7- Hemolytic uremic syndrome: Escherichia coli O157:H7
8- Hemolytic anemia
CHRONIC DIARRHOEA
chronic or persistent diarrhea is defined as an episode that lasts longer than 14 days.
four principle pathophysiologic mechanisms: osmotic, secretory, dysmotility associated, and inflammatory
1- Osmotic diarrhea is caused by a failure to absorb a luminal solute, resulting in secretion of fluids and net water retention across an osmotic gradient(best exemplified by the common disorder of lactose malabsorption) , either because of dissacharidase deficiencies or because the absorptive capacity of the intestine for that sugar may be overwhelmed by excessive consumption, eg, fructose and sorbitol. Such excessive intake may be seen in young children drinking fruit juices
2- Secretory diarrhea occurs when there is a net secretion of electrolyte and fluid from the intestine without compensatory absorption, Children with a pure secretory diarrhea will therefore continue to experience diarrhea even while fasting. (Congenital chloride diarrhea)
3- Chronic diarrhea associated with intestinal dysmotility typically occurs in the setting of intact absorptive abilities. Intestinal transit time is decreased, the time allowed for absorption is minimized, and fluid is retained within the lumen(diarrhea-predominant irritable bowel syndrome (IBS))
4- Inflammatory diarrhea (may encompass all of the pathophysiologic mechanisms) . Inflammation with resultant injury to the intestine may lead to malabsorption of dietary macronutrients which, in turn, creates a luminal osmotic gradient. Additionally, particular infectious agents may induce secretion of fluid into the lumen, and blood in the gut may alter intestinal motility. Diseases such as inflammatory bowel disease (IBD) and celiac disease
four principle pathophysiologic mechanisms: osmotic, secretory, dysmotility associated, and inflammatory
1- Osmotic diarrhea is caused by a failure to absorb a luminal solute, resulting in secretion of fluids and net water retention across an osmotic gradient(best exemplified by the common disorder of lactose malabsorption) , either because of dissacharidase deficiencies or because the absorptive capacity of the intestine for that sugar may be overwhelmed by excessive consumption, eg, fructose and sorbitol. Such excessive intake may be seen in young children drinking fruit juices
2- Secretory diarrhea occurs when there is a net secretion of electrolyte and fluid from the intestine without compensatory absorption, Children with a pure secretory diarrhea will therefore continue to experience diarrhea even while fasting. (Congenital chloride diarrhea)
3- Chronic diarrhea associated with intestinal dysmotility typically occurs in the setting of intact absorptive abilities. Intestinal transit time is decreased, the time allowed for absorption is minimized, and fluid is retained within the lumen(diarrhea-predominant irritable bowel syndrome (IBS))
4- Inflammatory diarrhea (may encompass all of the pathophysiologic mechanisms) . Inflammation with resultant injury to the intestine may lead to malabsorption of dietary macronutrients which, in turn, creates a luminal osmotic gradient. Additionally, particular infectious agents may induce secretion of fluid into the lumen, and blood in the gut may alter intestinal motility. Diseases such as inflammatory bowel disease (IBD) and celiac disease
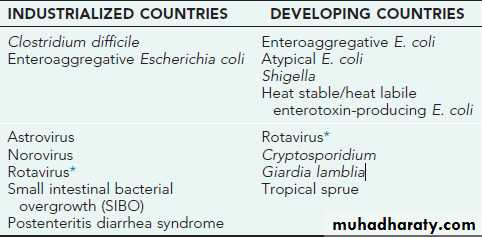
AETIOLOGY
1- Enteric infections are by far the most frequent cause of chronic diarrhea, both in developing and industrialized countries
2- Lactose intolerance or carbohydrate malabsorption may be caused by a brush-border enzyme defect in lactase or other enzymes--More commonly, lactose intolerance is secondary to lactase deficiency caused by intestinal mucosal damage.
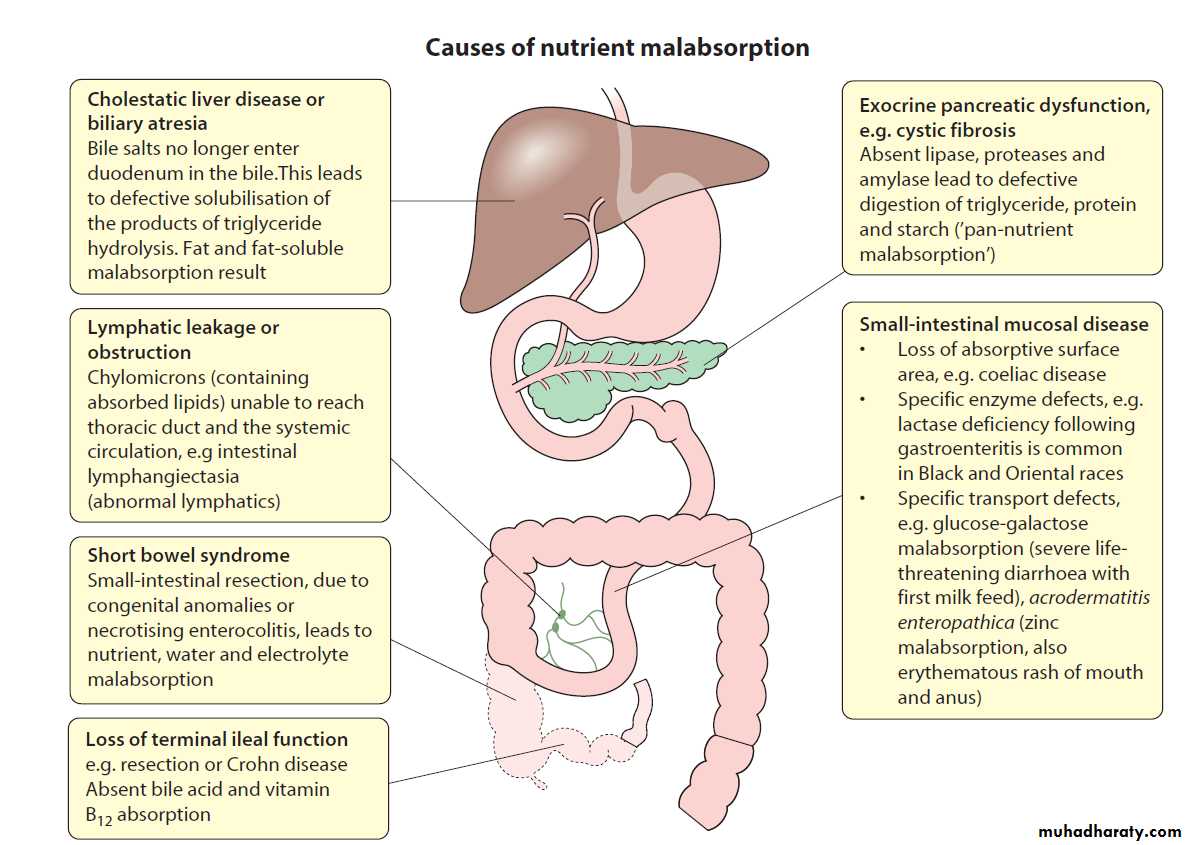
3- Allergy to cow’s milk protein and other food proteins also may present during infancy with chronic diarrhea
4- Chronic diarrhea may be the manifestation of maldigestion caused by exocrine pancreatic disorders. In most patients with cystic fibrosis, exocrine pancreatic insufficiency results in steatorrhea and protein malabsorption
5- The most benign etiology of chronic diarrhea is nonspecific diarrhea that encompasses functional diarrhea (or toddler’s diarrhea) in children younger than 4 yr of age and irritable bowel syndrome in those 5 yr of age and older. The diseases fall under the umbrella of functional disorders, in that in older children abdominal pain is often associated with diarrhea alternating with constipation and growth and weight gain are normal
6- In older children and adolescents, inflammatory bowel diseases, including Crohn disease, ulcerative colitis cause chronic diarrhea that is often associated with abdominal pain, elevated inflammatory markers
7- Diarrhea may be the result from an excessive intake of fluid and carbohydrate(fruit juice). If the child’s fluid intake were >150 mL/kg/24 hr, fluid intake should be reduced not to exceed 90 mL/kg/24 hr
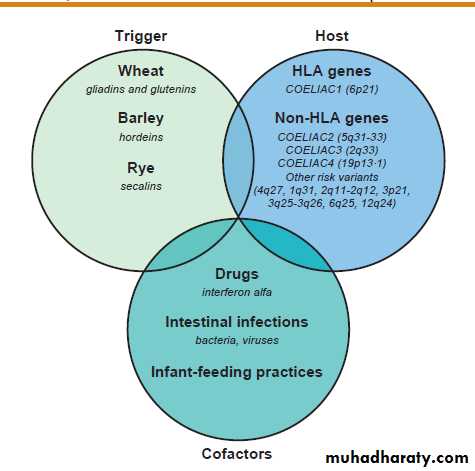
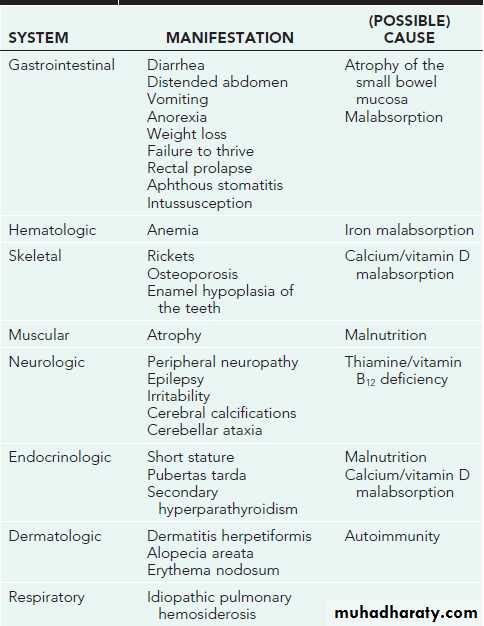
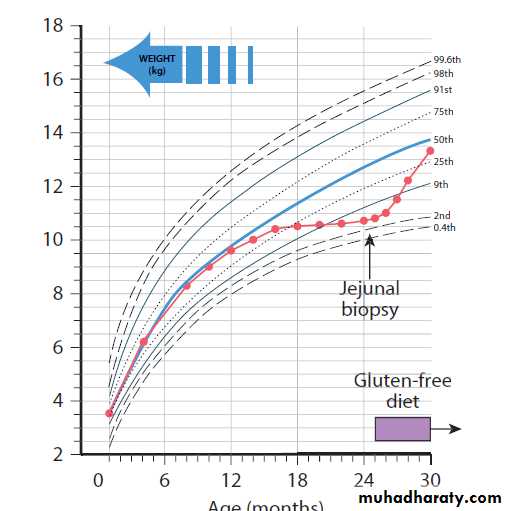
8- A reduction of intestinal absorptive surface is responsible for diarrhea in celiac disease, a genetically determined permanent gluten intolerance that affects as many as 1 in 100 individuals, depending on geographic origin. In the genetically susceptible host, gliadin, the major protein of gluten, reacts with the immune system to cause villous atrophy. The reduction of functional absorptive surface area is reversible upon restriction of gluten from the diet.
DIAGNOSIS
The diagnosis of celiac disease is based on a combination of symptoms,antibodies, HLA, and duodenal histology
TREATMENT
The only treatment for celiac disease is lifelong strict adherence to a gluten-free diet .This requires a wheat-, barley-, and rye-free diet
Malabsorption
Disorders affecting the digestion or absorption of nutrients
manifest as:
• abnormal stools(The true malabsorption stool is difficult to flush down the toilet and has an odor which pervades the whole house,pale,bulky)
• failure to thrive or poor growth in most but not all cases
• specific nutrient deficiencies, either singly or in combination.
manifest as:
• abnormal stools(The true malabsorption stool is difficult to flush down the toilet and has an odor which pervades the whole house,pale,bulky)
• failure to thrive or poor growth in most but not all cases
• specific nutrient deficiencies, either singly or in combination.
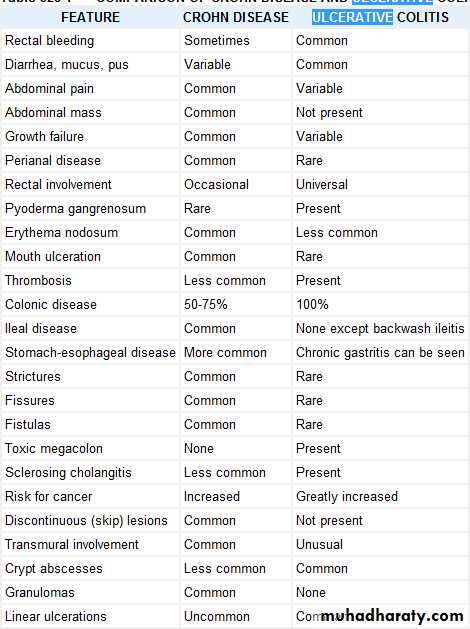
Inflammatory bowel disease
Approximately a quarter of patients present in childhood or adolescence. Crohn disease can affect any part of the gastrointestinal tract from mouth to anus, whereas in ulcerative colitis the inflammation is confined to the colon
Ulcerative colitis
Diagnosis:
made on endoscopy (upper and ileocolonoscopy) and on the histological features, after exclusion of infective causes of colitis
In contrast to adults, in whom the colitis is usually confined to the distal colon, 90% of children have a pancolitis
made on endoscopy (upper and ileocolonoscopy) and on the histological features, after exclusion of infective causes of colitis
In contrast to adults, in whom the colitis is usually confined to the distal colon, 90% of children have a pancolitis
TREATMENT
In mild disease, aminosalicylates (balsalazide and mesalazine) are used for induction and maintenance therapy. Disease confined to the rectum and sigmoid colon may be managed with topical steroids
More aggressive or extensive disease requires systemic steroids for acute exacerbations and immunomodulatory therapy, e.g. azathioprine to maintain remission alone or in combination with low-dose corticosteroid therapy.
More aggressive or extensive disease requires systemic steroids for acute exacerbations and immunomodulatory therapy, e.g. azathioprine to maintain remission alone or in combination with low-dose corticosteroid therapy.
CRONH DIASEASE
Diagnosis is based on endoscopic and histological findings on biopsy. Upper gastrointestinal endoscopy, ileocolonoscopy and small bowel imaging are required.
TREATMENT : Remission is induced with nutritional therapy, when the normal diet is replaced by whole protein modular feeds (polymeric diet) for 6–8 weeks. This is effective in 75% of cases. Systemic steroids are required if ineffective.
TREATMENT : Remission is induced with nutritional therapy, when the normal diet is replaced by whole protein modular feeds (polymeric diet) for 6–8 weeks. This is effective in 75% of cases. Systemic steroids are required if ineffective.
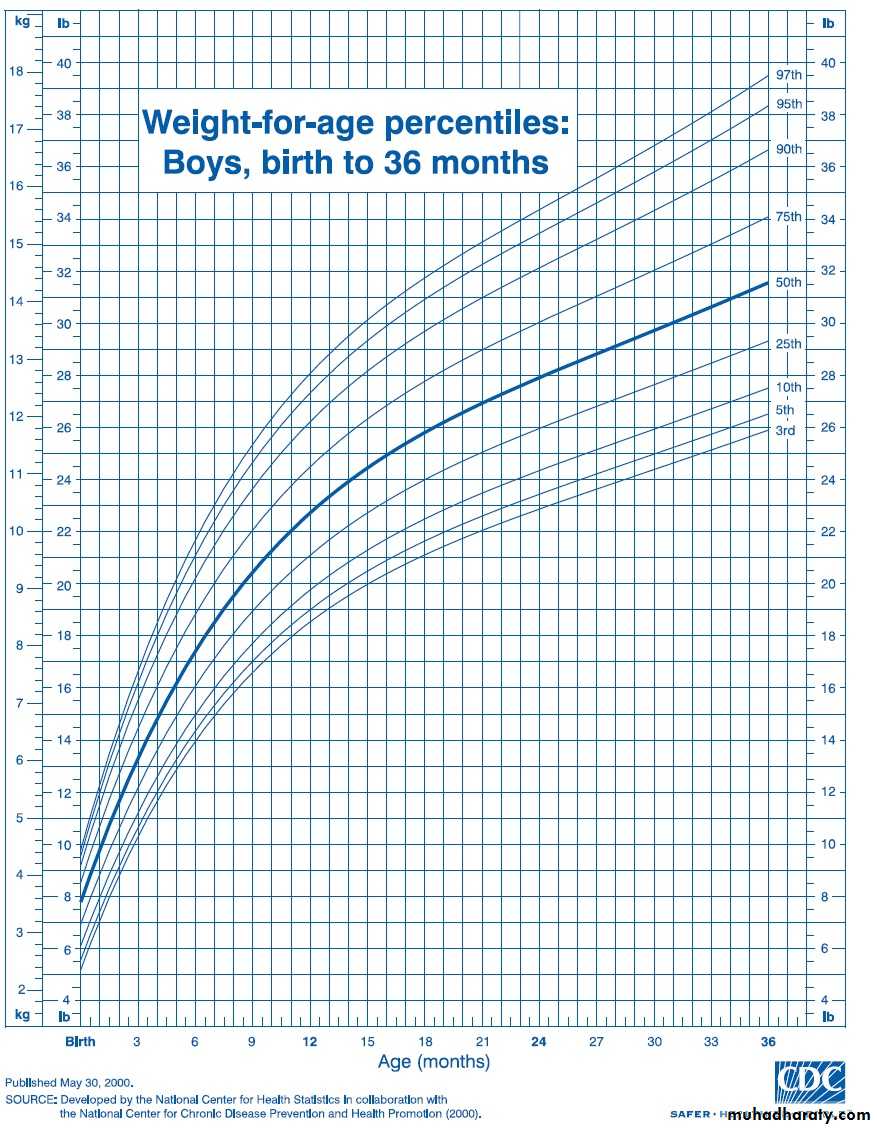
Failure to thrive(FTT)
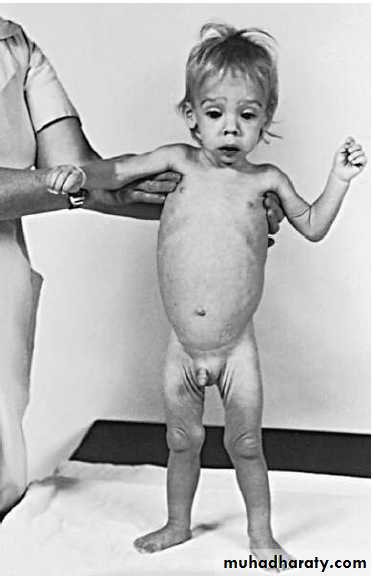
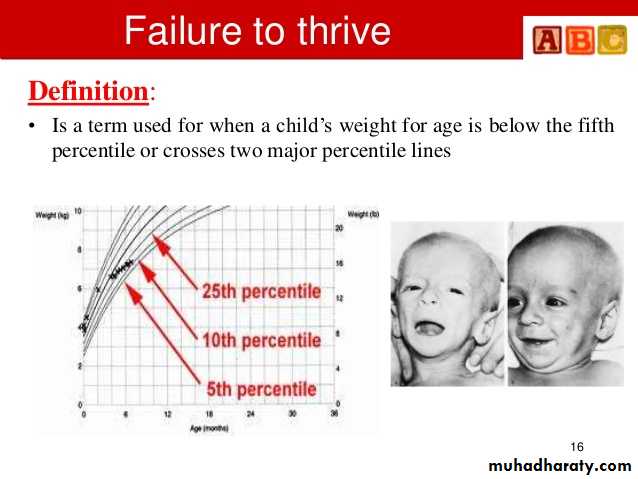
The term ‘failure to thrive’ is used to describe suboptimal, weight gain in infants and toddlers (malnourished infants and young children who fail to meet expected standards of growth).
FTT is a common problem in pediatrics, affecting 5% to 10% of young children and approximately 3% to 5% of children admitted to hospitals.
FTT is more common in children living in poverty and foster care and affects 15% of these group
FTT is a common problem in pediatrics, affecting 5% to 10% of young children and approximately 3% to 5% of children admitted to hospitals.
FTT is more common in children living in poverty and foster care and affects 15% of these group
OTHER DEFINITIONS
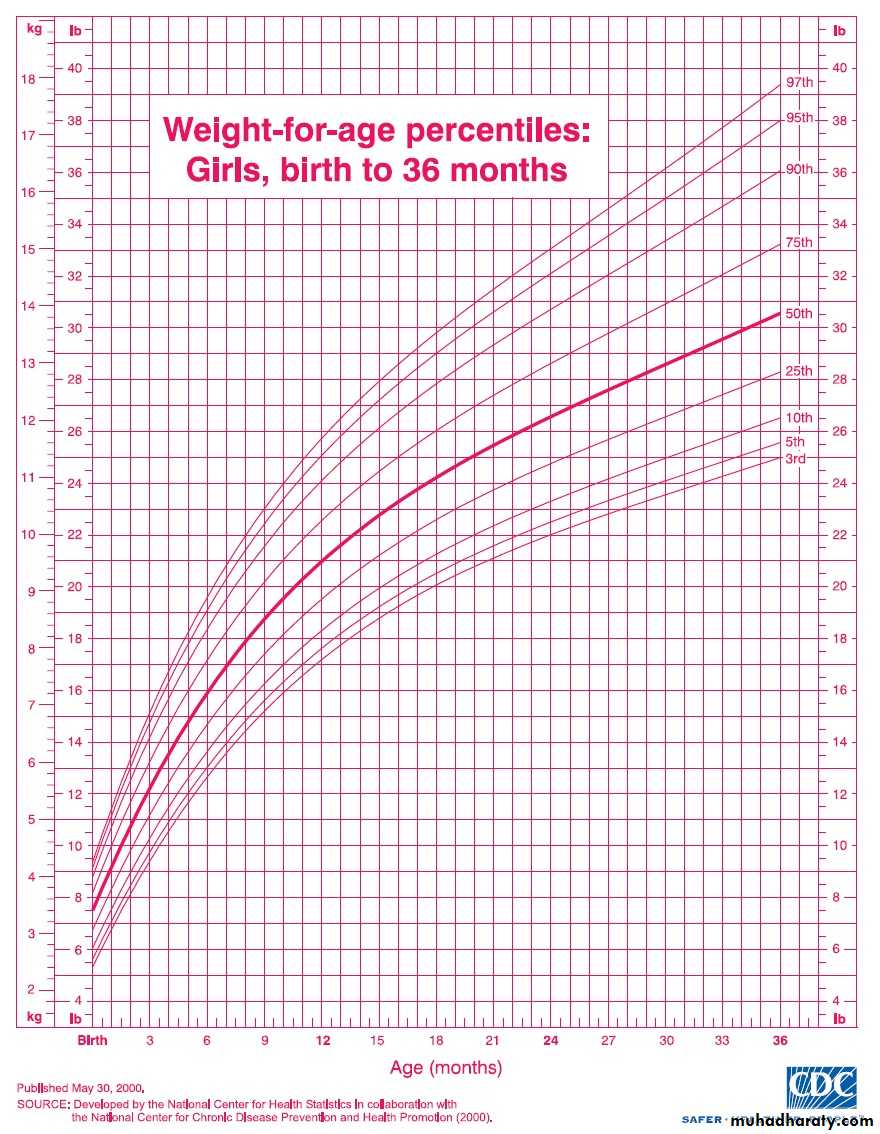
• weight that falls or remains below the 5th percentile for age.
• weight that decreases crossing two major percentile lines on the growth chart over time, (i.e., from above the 75th percentile to below the 25th)
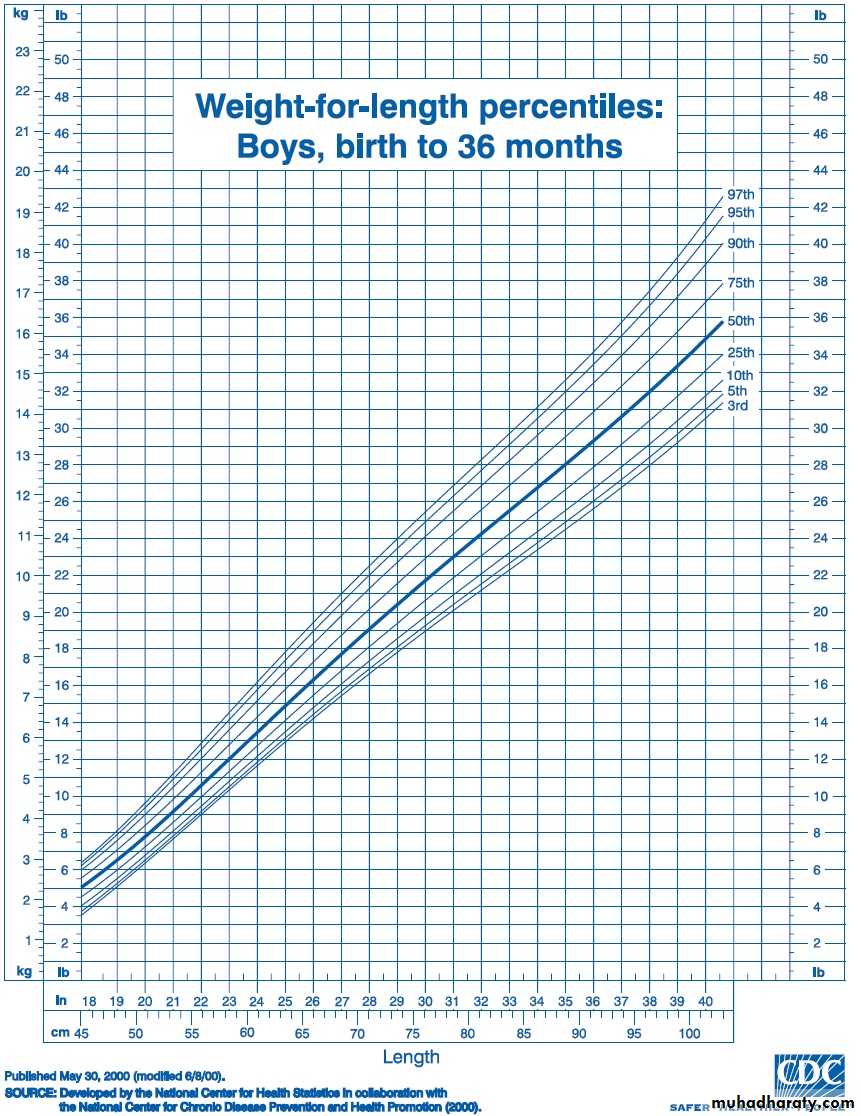
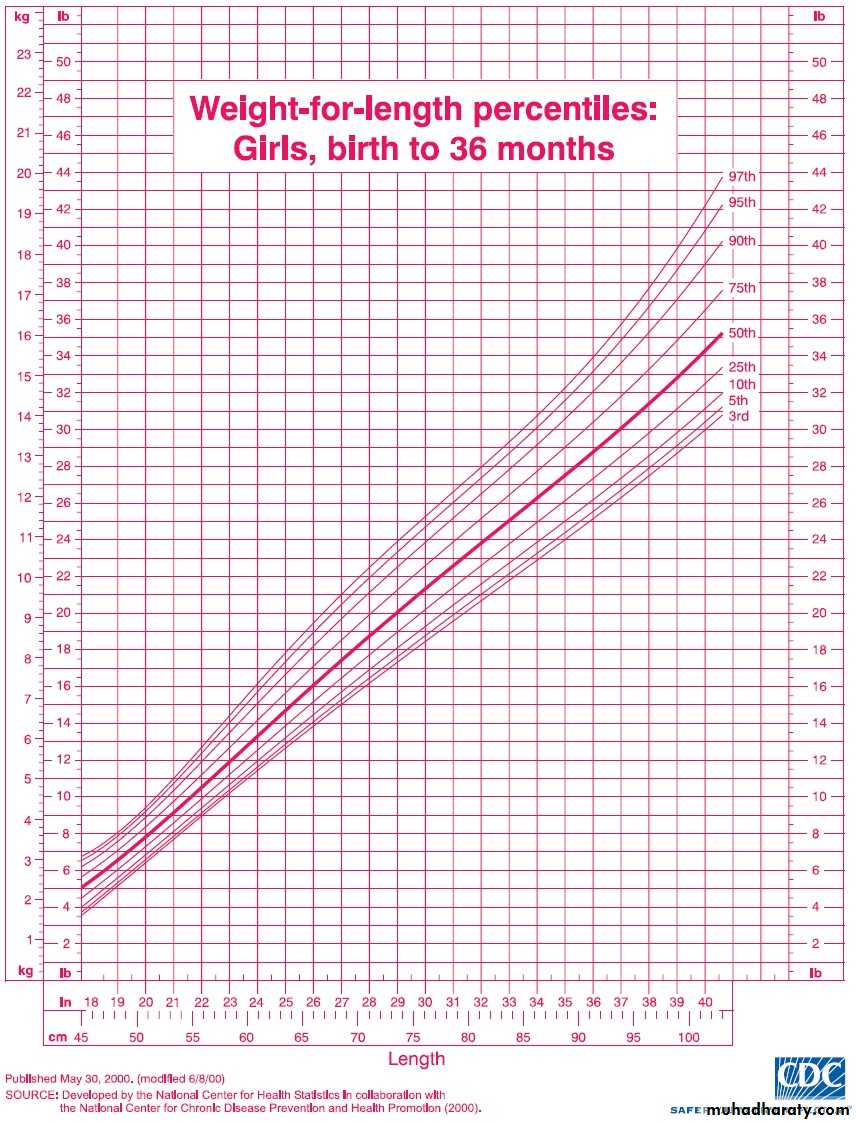
• weight that is less than 80% of the median weight for the height of the child
• weight that decreases crossing two major percentile lines on the growth chart over time, (i.e., from above the 75th percentile to below the 25th)
• weight that is less than 80% of the median weight for the height of the child
Repeated observations are therefore essential and are usually available from the child’s personal child health record
In children with FTT, malnutrition initially results in:
Wasting (deficiency in weight gain). then
Stunting (deficiency in linear growth) generally occurs after months of malnutrition.
Head circumference generally is spared except with chronic, severe malnutrition.
• Weight for height below the 5th percentile remains the single best growth chart indicator of acute undernutrition
• Children with chronic malnutrition often have a normal weight for height because both their weight and height are reduced.
Stunting (deficiency in linear growth) generally occurs after months of malnutrition.
Head circumference generally is spared except with chronic, severe malnutrition.
• Weight for height below the 5th percentile remains the single best growth chart indicator of acute undernutrition
• Children with chronic malnutrition often have a normal weight for height because both their weight and height are reduced.
Causes of FTT:
Organic FTT is marked by an underlying medical condition
Non organic or psychosocial FTT:
• It is far more common than organic FTT.
• Psychosocial FTT is most often due to poverty or poor child-parent interaction.
• Causes of Non organic (psychosocial FTT):
• Lack of food ( poverty)
• Lack of knowledge, (poor feeding techniques ,improper formula preparation, improper mealtime environment)
• Parental depression ,emotional deprivation, Child abuse or neglect .
• Psychosocial FTT is most often due to poverty or poor child-parent interaction.
• Causes of Non organic (psychosocial FTT):
• Lack of food ( poverty)
• Lack of knowledge, (poor feeding techniques ,improper formula preparation, improper mealtime environment)
• Parental depression ,emotional deprivation, Child abuse or neglect .
Organic Causes of Failure to Thrive:
Any chronic disease may lead to FTT
Gastrointestinal: GER, celiac disease, pyloric stenosis, cleft lip/ palate, lactose intolerance, Hirschsprung's disease, milk protein intolerance, hepatitis, cirrhosis, pancreatic insufficiency, biliary disease, inflammatory bowel disease, malabsorption
Renal: UTI, RTA, DI, RF
Cardiopulmonary: Cardiac diseases leading to CHF, asthma, BPD, CF, anatomic abnormalities of the upper airway,
Endocrine: Hyperthyroidism, DM, adrenal insufficiency or excess, parathyroid disorders, pituitary disorders,
Neurologic: MR, CP, degenerative disorders, CNS tumors
Infectious: Parasitic or bacterial infections of the gastrointestinal tract, TB, HIV disease
Metabolic: IEM
Genetics, Congenital: Chromosomal abnormalities, congenital syndromes (fetal alcohol syndrome), perinatal infections
Miscellaneous :Lead poisoning, malignancy, collagen vascular disease, recurrently infected adenoids and tonsils
Gastrointestinal: GER, celiac disease, pyloric stenosis, cleft lip/ palate, lactose intolerance, Hirschsprung's disease, milk protein intolerance, hepatitis, cirrhosis, pancreatic insufficiency, biliary disease, inflammatory bowel disease, malabsorption
Renal: UTI, RTA, DI, RF
Cardiopulmonary: Cardiac diseases leading to CHF, asthma, BPD, CF, anatomic abnormalities of the upper airway,
Endocrine: Hyperthyroidism, DM, adrenal insufficiency or excess, parathyroid disorders, pituitary disorders,
Neurologic: MR, CP, degenerative disorders, CNS tumors
Infectious: Parasitic or bacterial infections of the gastrointestinal tract, TB, HIV disease
Metabolic: IEM
Genetics, Congenital: Chromosomal abnormalities, congenital syndromes (fetal alcohol syndrome), perinatal infections
Miscellaneous :Lead poisoning, malignancy, collagen vascular disease, recurrently infected adenoids and tonsils
DIAGNOSIS AND CLINICAL MANIFESTATIONS
• History
• prenatal and postnatal factors :
• That influence growth, including the history of prenatal care, maternal illnesses during pregnancy, to
• Identify fetal growth problems (IUGR), birth size (weight, length, and head circumference).
• Identify prematurity
• Indicators of medical diseases (review of systems):
• such as vomiting, diarrhea, fever, respiratory symptoms, etc
• Careful dietary history is essential:
• The adequacy of the maternal milk supply or the precise preparation of formula should be evaluated.
• For older infants and young children, a detailed diet history is helpful,
• it is essential to evaluate intake of solid foods and liquids. Because of parental dietary beliefs, some children have inappropriately restricted diets. Other children with FTT drink excessive amounts of fruit juice, leading to malabsorption or anorexia for more nutrient-dense foods..
Social environment: poverty, unemployment, conflict , disruptive parent-child interactions
• prenatal and postnatal factors :
• That influence growth, including the history of prenatal care, maternal illnesses during pregnancy, to
• Identify fetal growth problems (IUGR), birth size (weight, length, and head circumference).
• Identify prematurity
• Indicators of medical diseases (review of systems):
• such as vomiting, diarrhea, fever, respiratory symptoms, etc
• Careful dietary history is essential:
• The adequacy of the maternal milk supply or the precise preparation of formula should be evaluated.
• For older infants and young children, a detailed diet history is helpful,
• it is essential to evaluate intake of solid foods and liquids. Because of parental dietary beliefs, some children have inappropriately restricted diets. Other children with FTT drink excessive amounts of fruit juice, leading to malabsorption or anorexia for more nutrient-dense foods..
Social environment: poverty, unemployment, conflict , disruptive parent-child interactions
• Physical examination :
• Growth chart: weight, height, OFC
• Systemic examination:
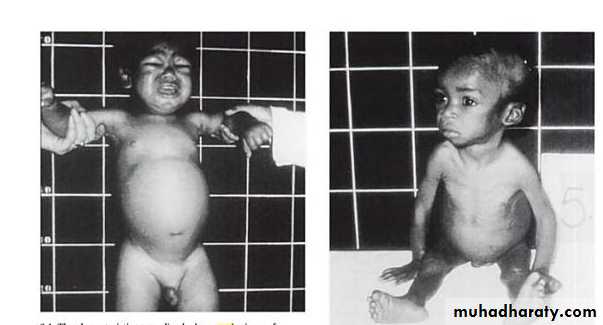
• Physical findings related to malnutrition, such as dermatitis, pallor, or edema
• Additionally, severely malnourished children are at risk for a variety of infections.
Depending on severity, the infant with FTT may exhibit thin extremities, a narrow face, prominent ribs, and wasted buttocks. Neglect of hygiene may be evidenced by diaper rash, unwashed skin, untreated impetigo, uncut and dirty fingernails, or unwashed clothing. A flattened occiput with hair loss may indicate that the child has been lying on his or her back. This flattening may be due to being unattended for prolonged periods. Delays in social and speech development are common. Other findings may include an avoidance of eye contact, an expressionless face, hypotonia, and the absence of a cuddling response.
• Systemic examination:
• Physical findings related to malnutrition, such as dermatitis, pallor, or edema
• Additionally, severely malnourished children are at risk for a variety of infections.
Depending on severity, the infant with FTT may exhibit thin extremities, a narrow face, prominent ribs, and wasted buttocks. Neglect of hygiene may be evidenced by diaper rash, unwashed skin, untreated impetigo, uncut and dirty fingernails, or unwashed clothing. A flattened occiput with hair loss may indicate that the child has been lying on his or her back. This flattening may be due to being unattended for prolonged periods. Delays in social and speech development are common. Other findings may include an avoidance of eye contact, an expressionless face, hypotonia, and the absence of a cuddling response.
• Laboratory evaluation:
• There is no need for extensive laboratory search for medical diseases
• Simple screening tests are recommended to screen for the common illnesses that may cause growth failure and to search for medical problems that result from malnutrition.
• Recommended laboratory tests include:
• CBP : type of anemia, WBC abnormalities (leucocytosis, lymphopenia)
• Urinalysis, urine culture: UTI
• Serum electrolytes & RFT
• Serum protein: Degree of protein deficiency
• Blood sugar: hpoglycemia
• Stool sample for culture and ova and parasites may be indicated for children with diarrhea, abdominal pain, or malodorous stools.
• PPD: screen for TB
• Simple screening tests are recommended to screen for the common illnesses that may cause growth failure and to search for medical problems that result from malnutrition.
• Recommended laboratory tests include:
• CBP : type of anemia, WBC abnormalities (leucocytosis, lymphopenia)
• Urinalysis, urine culture: UTI
• Serum electrolytes & RFT
• Serum protein: Degree of protein deficiency
• Blood sugar: hpoglycemia
• Stool sample for culture and ova and parasites may be indicated for children with diarrhea, abdominal pain, or malodorous stools.
• PPD: screen for TB
TREATMENT
Most children with FTT can be treated in the outpatient setting.
Hospitalization is required for
Children with severe malnutrition.
Children with underlying diagnoses that require hospitalization for evaluation or treatment.
Children whose safety is in danger because of maltreatment( social issues of the family).
Nutritional management:
It is the cornerstone of treatment of FTT, regardless of the etiology.
In general, the simplest and least costly approach to dietary change is warranted.
Amount:
• SLOW GRADUAL INCREMENT
• The final target is to provide 100 to 120 kcal/kg based on ideal weight.
Type:
• according to age of the child & type of feeding :
• Breast fed infant: continue breast feeding and may add cow milk or special cows’ milk based formula (F75 or F100).
• Bottle fed :
• Increased amount of cow milk ,or change to other types if indicated like:
• special cows’ milk based formula(F75 or F100)
• calorically dense formula (for anorectic and picky eater) concentration of formula can be changed from 20 cal/oz to 24 or 27 cal/oz
• soy based (isomil) for lactose-intolerant child
• hydrolyzed protein type (pregestemil) for cow milk protein intolerant
• home made (oil,butter,peanut butter, others)
• Toddlers:
• Dietary changes should include increasing the caloric density of favorite foods by adding butter, oil, peanut butter, or other high-calorie foods.
• High-calorie oral supplements that provide 30 cal/oz are often well tolerated by toddlers.
• The final target is to provide 100 to 120 kcal/kg based on ideal weight.
Type:
• according to age of the child & type of feeding :
• Breast fed infant: continue breast feeding and may add cow milk or special cows’ milk based formula (F75 or F100).
• Bottle fed :
• Increased amount of cow milk ,or change to other types if indicated like:
• special cows’ milk based formula(F75 or F100)
• calorically dense formula (for anorectic and picky eater) concentration of formula can be changed from 20 cal/oz to 24 or 27 cal/oz
• soy based (isomil) for lactose-intolerant child
• hydrolyzed protein type (pregestemil) for cow milk protein intolerant
• home made (oil,butter,peanut butter, others)
• Toddlers:
• Dietary changes should include increasing the caloric density of favorite foods by adding butter, oil, peanut butter, or other high-calorie foods.
• High-calorie oral supplements that provide 30 cal/oz are often well tolerated by toddlers.
Vitamin and mineral supplementation:
• It is needed, especially during catch-up growth. Vitamin and mineral intake in excess of the daily recommended intake is provided to account for the increased requirements; this is frequently accomplished by giving an age-appropriate daily multiple vitamin.


















Comments
Post a Comment