Pediatirc Nephtology/ Nephrotic Syndrome
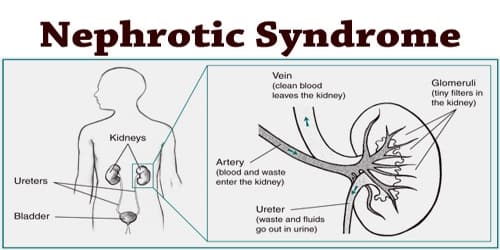
Nephrotic syndrome is defined by the clinical findings of heavy proteinuria, hypoalbuminemia,generalized edema and hyperlipidemia.
Minimal change nephrotic syndrome Focal segmental glomerulosclerosis Mesangial hypercellularity Membranoproliferative glomerulonephritis Membranous nephropathy
More than 80% of children under 7 years of age with nephrotic syndrome have MCNS. Children 7 to 16 years old with NS have a 50% chance of having MCNS, and males are affected more frequently than females (2:1).
The male-to-female ratio is reported to be 2:1 for children and 1:1 in adolescents and adults. most of minimal change nephrotic syndrome (MCNS)
have remission of their disease with a course ofprednisone.
Clothing may be tight and socks may leave indentations in the skin of the shins and ankles.
The abdomen may be distended, and a fluid wave may be discernible on examination.
Breath sounds may be decreased at the lungs bases because of accumulation of pleural fluid.
Although intravascular volume is low in most children with nephrotic syndrome, in some it will be increased. These latter children may present with a gallop on auscultation of the heart, rales over the lung fields, and hepatomegaly
The child or parents may report decreased frequency of urination and the passage of a dark, amber-colored, concentrated-appearing urine that appears to foam when voided into the toilet. Overall, 16% of children with nephrotic syndrome have diastolic hypertension on presentation. The presence of significant hypertension should raise the possibility of underlying glomerulonephritis.
Urinary protein losses can be quantified with a 24-hour urine collection
Nephrotic-range proteinuria is defined as (1) urinary protein excretion on a timed urine collection of greater than 2 g/day or greater than 40mg per M 2 per hr. Proteinuria of 1+ or higher on two to three random urine specimens suggests persistent proteinuria that should be further quantified.
Urinary protein quantification is not critical in the management of the nephrotic child who has heavy proteinuria as demonstrated by dipstick (+3 or+4 )determination and a typical clinical presentation. It is more helpful for following the response of children with resistant forms of nephrotic syndrome.
A small amount of protein is found in the urine of healthy children (<4 mg/m2/hour or UPr/Cr < 0.2).
Nephrotic proteinuria in children is defined as protein greater than 40 mg/m2/hour or UPr/Cr greater than 2.0. Proteinuria between these two levels is mildly to moderately elevated, but not nephrotic.
The presence of significant microscopic hematuria or gross hematuria should suggest that nephrotic syndrome might be secondary to an underlying nephritic process. The presence of glycosuria in untreated children with nephrotic syndrome suggests underlying tubular injury that may be seen with focal segmental glomerulosclerosis.
Blood urea and creatinine values generally are normal or only slightly elevated in primary nephrotic syndrome.
Serum total protein and albumin levels are low.
Mild hyponatremia may be present because of water retention.
Total calcium levels are low because of the low serum albumin level, but ionized calcium levels usually are normal.
The serum cholesterol level usually is elevated.
The third component of complement generally is normal. A depressed level suggests membranoproliferative glomerulonephritis, poststreptococcal glomerulonephritis, or lupus nephritis.
Chest radiographs usually will show a small cardiac silhouette and, in severe cases, the presence of pleural fluid. Cardiomegaly may be seen in those cases with increased intravascular volume.
Morbidity and mortality were high in nephrotic syndrome before the introduction of corticosteroids and antibiotics.
Infection was the leading cause of death in children with nephrotic syndrome.
Staphylococcus and gram-negative bacteria are responsible for the majority of infections in nephrotic syndrome.
defective opsonization of invading bacteria caused by loss into the urine of small components of the alternative pathway of complement,
and impaired cellular immunity.
In addition, the effects of immunosuppressive therapies used in the treatment of nephrotic syndrome may increase the susceptibility to infection.
Children with recurrent nephrotic syndrome should receive multivalent pneumococcal vaccination. A role for prophylactic antibiotic therapy has not been established.
Contributory factors include elevated plasma levels of procoagulant factors, urinary loss of inhibitors of coagulation, and thrombocytosis.
The predisposition to thrombus formation may be exacerbated by decreased intravascular volume, especially in the face of vigorous forced diuresis.
In addition, in severe disease there may be decreased lipolysis, resulting in elevated triglycerides.
SPECIFIC HISTOPATHOLOGICAL ENTITIES ASSOCIATED WITH PRIMARY NEPHROTIC SYNDROME OF CHILDHOOD
Minimal Change Nephrotic Syndrome
is the most common pathological diagnosis in nephrotic children
and as noted previously, 92% will achieve a remission with a course of corticosteroids
Hematuria is found in about 13% and hypertension in 10% to 20%.
Often, the diagnosis is assumed in most children since biopsy generally is not performed in those who follow a typical course and respond to steroids.
These children should more correctly be considered to have the clinical diagnosis of steroid-responsive idiopathic nephrotic syndrome of childhood,
prednisone
.
Seventy-five percent of those who will respond do so within 2 weeks of starting corticosteroids, and 94% will have responded by 4 weeks.
The majority of steroid-responsive patients have MCNS. However, up to 25% of steroid-resistant nephrotic children have MCNS on biopsy, whereas 5% to 10% of the steroid-responsive patients have FSGS
In general, nephrotic patients who achieve a remission on steroids, whether they have MCNS or FSGS by biopsy, do not progress to renal failure if they remain steroid responsive.
Children between the ages of 1 and 6 years are most likely to have MCNS by renal biopsy and respond clinically to a trial of steroids by achieving a remission
Therefore, it is now customary to treat a child in this age range (or even up to age 10) who presents with the new onset of typical, pure nephrotic syndrome with a trial of corticosteroids
day (maximum 60 to 80 mg/day) for 4 to 6 weeks
. This usually is given in divided doses
for an additional 4 to 6 weeks given in the morning on alternate days.
with the medication gradually tapered off after that
Depending on the treatment regimen employed, from 36% to 61% of children will have a relapse of nephrotic syndrome within the first year of the initial episode.
A relapse is diagnosed if the urine tests 2+ or greater for protein for 3 consecutive days with edema
Relapses usually are triggered by intercurrent illnesses or allergies, and parents can be taught to use albumin test sticks or sulfosalicylic acid at home to monitor urinary protein excretion. Relapses are treated with prednisone 2
mg/kg/day or 60 mg/M
day until the urine is free of protein(negative or trace or+1)
for 3 consecutive days
That is in the same manner of the first episode.
About 25% of children with relapses will follow a frequently relapsing course, defined as 2 relapses occurring within 6 months of completing a course of steroids or 3 relapses within 1 year.
Children who develop a relapse while corticosteroids are being tapered or within 2 weeks of completing a course of steroids are considered to be steroid-dependent.
Both children who have frequently relapsing and steroid-dependent nephrotic syndrome are more likely to develop steroid toxicity. Secondary, tertiary, and complementary therapies for difficult cases of nephrotic syndrome are listed
Secondary, Tertiary, and Complementary Therapies for Difficult Cases of Nephrotic Syndrome
Cyclophosphamide Chlorambucil Cyclosporine Tacrolimus Methylprednisolone Levamisole Angiotensin-converting enzyme inhibitors Nonsteroidal antiinflammatory drugs
Children who fail to respond to the initial or subsequent courses of corticosteroids have steroid-resistant nephrotic syndrome and a more guarded prognosis.
Consultation with a pediatric nephrologist should be made for consideration of a renal biopsy and more aggressive treatment
can be associated with increased risk of infection,
malignancy, and sterility, but usually only with higher doses than those typically used for nephrotic syndrome or after repeated or prolonged courses. Cyclophosphamide can cause hemorrhagic cystitis. Therefore, a large fluid intake and frequent voiding should be encouraged. Chlorambucil therapy has been associated with induction of seizure activity.
Nonsteroidal antiinflammatory drugs can cause salt retention and edema. There is a risk of renal failure, especially in patients with severely decreased intravascular volume.
Diuretics are used judiciously given the already reduced intravascular volume in most nephrotic patients and the attendant risk of thromboembolism. Furosemide alone or in combination with a thiazide diuretic is used for significant edema. Severe edema interfering with ambulation, compromising respiratory status, or causing tissue breakdown can be treated with intravenous 25% albumin, 1 g/kg, followed by intravenous furosemide if renal function and urine output are fairly well maintained
can be tried in resistant nephrotic syndrome, even in the presence of normotension, to decrease urinary protein excretion. The ACE inhibitors act by decreasing glomerular capillary pressure and can cause a reversible rise in serum creatinine and hyperkalemia that must be monitored
Outside the expected age range (younger than 1 year old or older than10 years old
Accompanied by signs of glomerulonephritis (renal insufficiency, hypertension, hematuria, hypocomplementemia(
Refractory edema
Frequently relapsing nephrotic syndrome
Steroid-dependent nephrotic syndrome
Steroid-resistant nephrotic syndrome
Anasarca interfering with ambulation or compromising ventilation
Pleural effusions or ascites interfering with ventilation
Signs of volume overload (congestive heart failure(
Infection (e.g., severe cellulitis, peritonitis
Significant hypertension
Significant electrolyte abnormalities
Compromised renal function
EPIDEMIOLOGY
examples of Primary and Secondary CausesMinimal change nephrotic syndrome Focal segmental glomerulosclerosis Mesangial hypercellularity Membranoproliferative glomerulonephritis Membranous nephropathy
Secondary Nephrotic Syndrome
Minimal change nephrotic syndrome (MCNS) is the most common histologic form of primary nephrotic syndrome in children.More than 80% of children under 7 years of age with nephrotic syndrome have MCNS. Children 7 to 16 years old with NS have a 50% chance of having MCNS, and males are affected more frequently than females (2:1).
The male-to-female ratio is reported to be 2:1 for children and 1:1 in adolescents and adults. most of minimal change nephrotic syndrome (MCNS)
have remission of their disease with a course ofprednisone.
pathophysiology
Nephrotic syndrome (NS) is characterized by persistent heavy proteinuria (mainly albuminuria) (>2 g/24 hours); hypoproteinemia (serum albumin <3.0 g/dL); hypercholesterolemia (>250 mg/dL); and edema. Age, race, and geography affect the incidence of NS.pathophysiology
Certain HLA types (HLA-DR7, HLA-B8, and HLA-B12) are associated with an increased incidence of NS. The increased glomerular permeability to serum proteins is due to alterations in glomerular basement membrane proteins and their normal negative charge that restricts filtration of serum proteinspathophysiology
The resultant massive proteinuria leads to a decline in serum proteins, especially albumin. Plasma oncotic pressure is diminished, resulting in fluid shifts from the vascular to the interstitial compartment and plasma volume contraction..pathophysiology
Edema formation is enhanced by reduction in effective circulating blood volume and increase in tubular sodium chloride reabsorption secondary to activation of the renin-angiotensin-aldosterone systempathophysiology
Hypoproteinemia stimulates hepatic lipoprotein synthesis and diminishes lipoprotein metabolism, leading to elevated serum lipids (cholesterol, triglycerides) and lipoproteinsPRESENTATION
signs &symptomstypically presents with the gradual development of edema and inappropriate weight gain
The presence of periorbital edema upon arising in the morning that resolve during the course of the day often is mistaken for allergy.Clothing may be tight and socks may leave indentations in the skin of the shins and ankles.
The abdomen may be distended, and a fluid wave may be discernible on examination.
Breath sounds may be decreased at the lungs bases because of accumulation of pleural fluid.
Although intravascular volume is low in most children with nephrotic syndrome, in some it will be increased. These latter children may present with a gallop on auscultation of the heart, rales over the lung fields, and hepatomegaly
The child or parents may report decreased frequency of urination and the passage of a dark, amber-colored, concentrated-appearing urine that appears to foam when voided into the toilet. Overall, 16% of children with nephrotic syndrome have diastolic hypertension on presentation. The presence of significant hypertension should raise the possibility of underlying glomerulonephritis.
LABORATORY EVALUATION
Laboratory evaluation begins with a urinalysis in the child with edema. This will demonstrate significant proteinuria in cases of nephrotic syndrome.Urinary protein losses can be quantified with a 24-hour urine collection
Nephrotic-range proteinuria is defined as (1) urinary protein excretion on a timed urine collection of greater than 2 g/day or greater than 40mg per M 2 per hr. Proteinuria of 1+ or higher on two to three random urine specimens suggests persistent proteinuria that should be further quantified.
Urinary protein quantification is not critical in the management of the nephrotic child who has heavy proteinuria as demonstrated by dipstick (+3 or+4 )determination and a typical clinical presentation. It is more helpful for following the response of children with resistant forms of nephrotic syndrome.
A small amount of protein is found in the urine of healthy children (<4 mg/m2/hour or UPr/Cr < 0.2).
Nephrotic proteinuria in children is defined as protein greater than 40 mg/m2/hour or UPr/Cr greater than 2.0. Proteinuria between these two levels is mildly to moderately elevated, but not nephrotic.
The presence of significant microscopic hematuria or gross hematuria should suggest that nephrotic syndrome might be secondary to an underlying nephritic process. The presence of glycosuria in untreated children with nephrotic syndrome suggests underlying tubular injury that may be seen with focal segmental glomerulosclerosis.
Blood urea and creatinine values generally are normal or only slightly elevated in primary nephrotic syndrome.
Serum total protein and albumin levels are low.
Mild hyponatremia may be present because of water retention.
Total calcium levels are low because of the low serum albumin level, but ionized calcium levels usually are normal.
The serum cholesterol level usually is elevated.
The third component of complement generally is normal. A depressed level suggests membranoproliferative glomerulonephritis, poststreptococcal glomerulonephritis, or lupus nephritis.
Chest radiographs usually will show a small cardiac silhouette and, in severe cases, the presence of pleural fluid. Cardiomegaly may be seen in those cases with increased intravascular volume.
COMPLICATIONS
InfectionMorbidity and mortality were high in nephrotic syndrome before the introduction of corticosteroids and antibiotics.
Infection was the leading cause of death in children with nephrotic syndrome.
Infectious complications include
spontaneous bacterial peritonitis, sepsis, cellulitis, and pneumoniae.Staphylococcus and gram-negative bacteria are responsible for the majority of infections in nephrotic syndrome.
Predisposing factors for the development of bacterial :infections include
tissue edema that may facilitate the spread of infection,defective opsonization of invading bacteria caused by loss into the urine of small components of the alternative pathway of complement,
and impaired cellular immunity.
In addition, the effects of immunosuppressive therapies used in the treatment of nephrotic syndrome may increase the susceptibility to infection.
Children with recurrent nephrotic syndrome should receive multivalent pneumococcal vaccination. A role for prophylactic antibiotic therapy has not been established.
Thromboembolism
Thromboembolic events such as deep-vein thrombosis, pulmonary embolism, and renal vein thrombosis are well-described complications of nephrotic syndrome in both childrenContributory factors include elevated plasma levels of procoagulant factors, urinary loss of inhibitors of coagulation, and thrombocytosis.
The predisposition to thrombus formation may be exacerbated by decreased intravascular volume, especially in the face of vigorous forced diuresis.
Hyperlipidemia
Elevated plasma cholesterol in nephrotic syndrome results from increased hepatic lipoprotein synthesis caused by generalized increased hepatic protein synthesis in response to a lowered plasma albumin level.In addition, in severe disease there may be decreased lipolysis, resulting in elevated triglycerides.
SPECIFIC HISTOPATHOLOGICAL ENTITIES ASSOCIATED WITH PRIMARY NEPHROTIC SYNDROME OF CHILDHOOD
Minimal Change Nephrotic Syndrome
Minimal change nephrotic syndrome (MCNS), also known as lipoid nephrosis
is the most common pathological diagnosis in nephrotic children
and as noted previously, 92% will achieve a remission with a course of corticosteroids
Hematuria is found in about 13% and hypertension in 10% to 20%.
Relapses are common, but the long-term prognosis is excellent.
Relapses tend to become less frequent with age, and the disorder usually resolves around the time of puberty without permanent renal impairment.Often, the diagnosis is assumed in most children since biopsy generally is not performed in those who follow a typical course and respond to steroids.
These children should more correctly be considered to have the clinical diagnosis of steroid-responsive idiopathic nephrotic syndrome of childhood,
MANAGEMENT
Eighty-five percent of nephrotic children regardless of underlying pathology will respond to a trial ofprednisone
.
Seventy-five percent of those who will respond do so within 2 weeks of starting corticosteroids, and 94% will have responded by 4 weeks.
The majority of steroid-responsive patients have MCNS. However, up to 25% of steroid-resistant nephrotic children have MCNS on biopsy, whereas 5% to 10% of the steroid-responsive patients have FSGS
In general, nephrotic patients who achieve a remission on steroids, whether they have MCNS or FSGS by biopsy, do not progress to renal failure if they remain steroid responsive.
Children between the ages of 1 and 6 years are most likely to have MCNS by renal biopsy and respond clinically to a trial of steroids by achieving a remission
Therefore, it is now customary to treat a child in this age range (or even up to age 10) who presents with the new onset of typical, pure nephrotic syndrome with a trial of corticosteroids
Treatment consists of
prednisone 2 mg/kg/day or 60 mg/Mday (maximum 60 to 80 mg/day) for 4 to 6 weeks
. This usually is given in divided doses
This is followed by a single dose of 2 mg/kg or 60
mg/Mfor an additional 4 to 6 weeks given in the morning on alternate days.
with the medication gradually tapered off after that
Depending on the treatment regimen employed, from 36% to 61% of children will have a relapse of nephrotic syndrome within the first year of the initial episode.
A relapse is diagnosed if the urine tests 2+ or greater for protein for 3 consecutive days with edema
Relapses usually are triggered by intercurrent illnesses or allergies, and parents can be taught to use albumin test sticks or sulfosalicylic acid at home to monitor urinary protein excretion. Relapses are treated with prednisone 2
mg/kg/day or 60 mg/M
day until the urine is free of protein(negative or trace or+1)
for 3 consecutive days
That is in the same manner of the first episode.
About 25% of children with relapses will follow a frequently relapsing course, defined as 2 relapses occurring within 6 months of completing a course of steroids or 3 relapses within 1 year.
Children who develop a relapse while corticosteroids are being tapered or within 2 weeks of completing a course of steroids are considered to be steroid-dependent.
Both children who have frequently relapsing and steroid-dependent nephrotic syndrome are more likely to develop steroid toxicity. Secondary, tertiary, and complementary therapies for difficult cases of nephrotic syndrome are listed
Secondary, Tertiary, and Complementary Therapies for Difficult Cases of Nephrotic Syndrome
Cyclophosphamide Chlorambucil Cyclosporine Tacrolimus Methylprednisolone Levamisole Angiotensin-converting enzyme inhibitors Nonsteroidal antiinflammatory drugs
Children who fail to respond to the initial or subsequent courses of corticosteroids have steroid-resistant nephrotic syndrome and a more guarded prognosis.
Consultation with a pediatric nephrologist should be made for consideration of a renal biopsy and more aggressive treatment
Side effects of treatment
significant complications of therapy include the development of cushingoid features, cataract formation, glaucoma, gastritis, peptic ulcer disease, pancreatitis, hypokalemia, hypertension, increased risk of infection, behavioral changes, and growth delay if treatment is prolonged.Cytotoxic agents
., cyclophosphamide, chlorambucil, nitrogen mustard, and cyclosporinecan be associated with increased risk of infection,
malignancy, and sterility, but usually only with higher doses than those typically used for nephrotic syndrome or after repeated or prolonged courses. Cyclophosphamide can cause hemorrhagic cystitis. Therefore, a large fluid intake and frequent voiding should be encouraged. Chlorambucil therapy has been associated with induction of seizure activity.
Nonsteroidal antiinflammatory drugs can cause salt retention and edema. There is a risk of renal failure, especially in patients with severely decreased intravascular volume.
Diuretics are used judiciously given the already reduced intravascular volume in most nephrotic patients and the attendant risk of thromboembolism. Furosemide alone or in combination with a thiazide diuretic is used for significant edema. Severe edema interfering with ambulation, compromising respiratory status, or causing tissue breakdown can be treated with intravenous 25% albumin, 1 g/kg, followed by intravenous furosemide if renal function and urine output are fairly well maintained
Angiotensin-converting enzyme (ACE) inhibitors (e.g
captopril enalaprilcan be tried in resistant nephrotic syndrome, even in the presence of normotension, to decrease urinary protein excretion. The ACE inhibitors act by decreasing glomerular capillary pressure and can cause a reversible rise in serum creatinine and hyperkalemia that must be monitored
When to Refer
Complicated nephrotic syndromeOutside the expected age range (younger than 1 year old or older than10 years old
Accompanied by signs of glomerulonephritis (renal insufficiency, hypertension, hematuria, hypocomplementemia(
Refractory edema
Frequently relapsing nephrotic syndrome
Steroid-dependent nephrotic syndrome
Steroid-resistant nephrotic syndrome
When to Hospitalize
Initial episode for teaching of parentsAnasarca interfering with ambulation or compromising ventilation
Pleural effusions or ascites interfering with ventilation
Signs of volume overload (congestive heart failure(
Infection (e.g., severe cellulitis, peritonitis
Significant hypertension
Significant electrolyte abnormalities
Compromised renal function

Comments
Post a Comment